Our Procedures
Cardiac AblationWhat Is Cardiac Ablation?
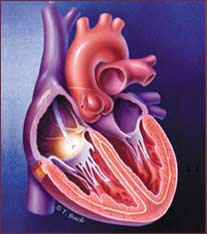
In cardiac ablation, a form of energy renders a small section of damaged tissue inactive. This puts an end to arrhythmias that originated at the problematic site.
Normally, electricity flows throughout the heart in a regular, measured pattern. This normally operating electrical system is the basis for heart muscle contractions.
Sometimes, the electrical flow gets blocked or travels the same pathways repeatedly creating something of a “short circuit” that disturbs normal heart rhythms. Medicine often helps. In some cases, however, the most effective treatment is to destroy the tissue housing the short circuit. This procedure is called cardiac ablation.
Cardiac ablation is just one of a number of terms used to describe the non-surgical procedure. Other common terms are: cardiac catheter ablation, radiofrequency ablation, cardiac ablation, or simply ablation.
The Ablation Process
Like many cardiac procedures, ablation no longer requires a full frontal chest opening. Rather, ablation is a relatively non-invasive procedure that involves inserting catheters – narrow, flexible wires – into a blood vessel, often through a site in the groin or neck, and winding the wire up into the heart. The journey from entry point to heart muscle is navigated by images created by a fluoroscope, an x-ray-like machine that provides continuous, “live” images of the catheter and tissue.
Once the catheter reaches the heart, electrodes at the tip of the catheter gather data and a variety of electrical measurements are made. The data pinpoints the location of the faulty electrical site. During this “electrical mapping,” the cardiac arrhythmia specialist, an electrophysiologist, may sedate the patient and instigate some of the very arrhythmias that are the crux of the problem. The events are safe, given the range of experts and resources close at hand, and are necessary to ensure the precise location of the problematic tissue.
Once the damaged site is confirmed, energy is used to destroy a small amount of tissue, ending the disturbance of electrical flow through the heart and restoring a healthy heart rhythm. This energy may take the form of radiofrequency energy, which cauterizes the tissue, or intense cold, which freezes, or cryoablates the tissue. Other energy sources are being investigated.
Patients rarely report pain, more often describing what they feel as discomfort. Some watch much of the procedure on monitors and occasionally ask questions. After the procedure, a patient remains still for four to six hours to ensure the entry point incision begins to heal properly. Once mobile again, patients may feel stiff and achy from lying still for hours.
When Is Ablation Appropriate
Many people have abnormal heart rhythms (arrhythmias) that cannot be controlled with lifestyle changes or medications. Some patients cannot or do not wish to take life-long antiarrhythmic medications and other drugs because of side effects that interfere with their quality of life.
Most often, cardiac ablation is used to treat rapid heartbeats that begin in the upper chambers, or atria, of the heart. As a group, these are know as supraventricular tachycardias, or SVTs. Types of SVTs are:
- Atrial Fibrillation
- Atrial Flutter
- AV Nodal Reentrant Tachycardia
- AV Reentrant Tachycardia
- Atrial Tachycardia
Less frequently, ablation can treat heart rhythm disorders that begin in the heart’s lower chambers, known as the ventricles. The most common, ventricular tachycardia, may also be the most dangerous type of arrhythmia because it can cause sudden cardiac death.
For patients at risk for sudden cardiac death, ablation often is used along with an implantable cardioverter device (ICD). The ablation decreases the frequency of abnormal heart rhythms in the ventricles and therefore reduces the number of ICD shocks a patient may experience.
For many types of arrhythmias, catheter ablation is successful in 90-98 percent of cases – thus eliminating the need for open-heart surgeries or long-term drug therapies.




